
12 The potential reduction on preload and afterload could reduce left ventricular wall stress and facilitate beneficial cardiac remodelling. The precise mechanisms by which SGLT2i reduces HHF are unclear but may involve natriuresis, reduction in interstitial oedema, reduced preload and afterload, improved renal function and cardio-renal physiology, inhibition of cardiac sodium-hydrogen exchange, and improved cardiac bioenergetics. This is likely to be the case since the Dapagliflozin in Patients With Heart Failure and Reduced Ejection Fraction (DAPA-HF) trial recently reported that dapagliflozin significantly reduced both the incidence of CVD and worsening heart failure in patients with heart failure with reduced ejection fraction, with and without T2D. 10 These consistent effects of SGLT2i glucose lowering therapy on HHF suggest the benefits may be a class effect and maybe independent of glycaemic control.

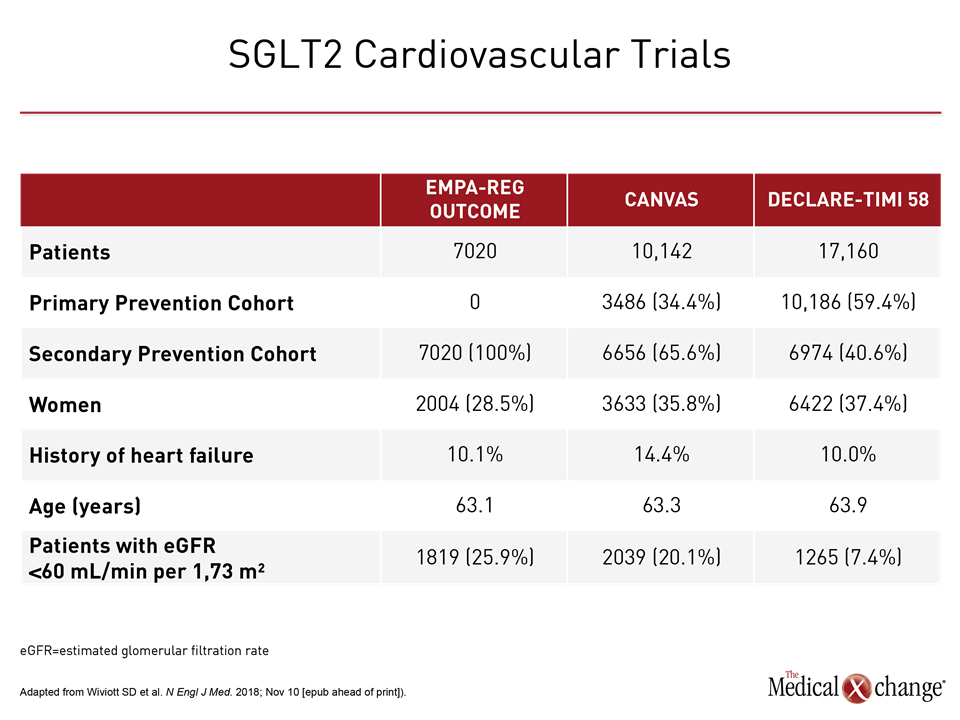
9 Significant reductions in HHF have also been reported for canagliflozin, in the Canagliflozin Cardiovascular Assessment Study (CANVAS) programme, trial. In the Dapagliflozin Effect on Cardiovascular Events (DECLARE TIMI 58) trial, treatment with dapagliflozin was non-inferior to placebo with respect to major adverse cardiovascular events but did result in a lower rate of the other pre-specified primary efficacy outcome (the composite of CVD or HHF) which reflected a lower rate of HHF. All-cause mortality was also reduced by 32%. 8 The most striking findings of this landmark trial were the profound early effects of the sodium-glucose cotransporter 2 inhibitor (SGLT2i), empagliflozin on CVD, and hospitalization for heart failure (HHF), which were reduced by 38% and 35%, respectively. 4–7 However, the recent Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients (EMPA-REG OUTCOME) trial was a landmark trial as it demonstrated for the first time that a glucose lowering agent could reduce CV events. Intensive management of hyperglycaemia in people with T2D using oral agents with or without insulin control reduces the risk of microvascular complications but appears to be insufficient to reduce cardiovascular (CV) events. Men with diabetes are twice as likely to have heart failure as those without T2D and women with T2D have a five-fold increased risk. 1, 2 Heart failure is an important manifestation of diabetic heart disease. Patients with type 2 diabetes (T2D) mellitus have double the risk of cardiovascular death (CVD) compared with people without T2D. See page 3433 for the editorial comment on this article (doi: 10.1093/eurheartj/ehaa530) Introduction Dapagliflozin significantly reduced pre-specified secondary endpoints including ambulatory 24-h systolic BP ( P = 0.012), nocturnal systolic BP ( P = 0.017), body weight ( P < 0.001), visceral adipose tissue (VAT) ( P < 0.001), subcutaneous adipose tissue (SCAT) ( P = 0.001), insulin resistance, Homeostatic Model Assessment of Insulin Resistance ( P = 0.017), and high-sensitivity C-reactive protein (hsCRP) ( P = 0.049).ĭapagliflozin, Heart failure, Left ventricular mass, Type 2 diabetes, Insulin resistance Additional sensitivity analysis adjusting for baseline LVM, baseline BP, weight, and systolic BP change showed the LVM change to remain statistically significant (mean change −2.92g 95% CI: −5.45 to −0.38, P = 0.025). In the intention-to-treat analysis, dapagliflozin significantly reduced LVM compared with placebo with an absolute mean change of −2.82g. Primary endpoint was change in absolute left ventricular mass (LVM), assessed by cardiac magnetic resonance imaging. We randomly assigned 66 people (mean age 67 ± 7 years, 38 males) with T2D, LVH, and controlled blood pressure (BP) to receive dapagliflozin 10 mg once daily or placebo for 12 months.


 0 kommentar(er)
0 kommentar(er)
